What is acute myeloid leukemia (AML)?
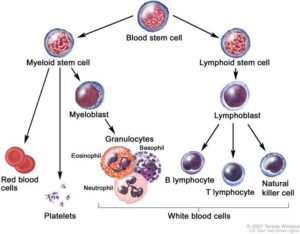
AML is a cancer of the blood in which the bone marrow makes too many immature myelocytes (white blood cells). All blood is made in the bone marrow where blood cells come from stem cells. Acute myeloid leukemia (AML) is a cancer of the white blood cells, where too many immature abnormal white blood cells, called “blasts”, are found in the bone marrow. There are numerous kinds of AML which were originally classified based on their appearance under the microscope. These blasts crowd out the normal blood cells in the bone marrow and spread to the blood. They can also spread to the brain, spinal cord, and/or other organs. Myeloblasts do not work like normal myeloid cells and are not able to fight infection. As the number of leukemia cells increases in the blood and bone marrow, there is less room for healthy red blood cells, and platelets which leads to anemia, and easy bleeding.
What are signs of childhood AML?
- Fever.
- Masses in the skull or other parts (chloroma)
- Easy bruising or bleeding.
- Bone or joint pain.
- Painless lumps in the neck, underarm, stomach, or groin.
- Pain or feeling of fullness below the ribs.
- Weakness, feeling tired, or looking pale.
What causes AML?
Nobody knows for sure, but commonly there is nothing in the environment or diet that caused this. Some cases of childhood AML are associated with genetic disorders such as Down Syndrome, Fanconi Anemia, and Kostmann Syndrome. Most cases and are not inherited so other children in the family should not be at risk, your doctor should be able to confirm that. It is not infectious so it cannot be passed onto other children or playmates.
How is AML diagnosed?
We may suspect the diagnosis from the blood count but the tests described below will confirm it and find out if leukemia has spread to other parts of the body e.g. spinal fluid
- Physical exam and history: An exam of the body to check or signs of disease, such as lumps or anything else that seems unusual e.g. testes enlargement.
- Blood tests: such as complete blood count (CBC) which tells the number and type of each blood cell, and blood chemistry studies because certain substances may be increased in acute leukemia.
- Bone marrow aspiration and biopsy: Removal of liquid bone marrow and a tiny piece of bone by inserting a needle into the hipbone while the child is sedated. A pathologist views the marrow sample under a microscope to look at the leukemia cells. Special tests done include flow cytometry to look at markers on the surface of the cells to confirm the diagnosis and subtype of AML and genetic analysis of the leukemia cells.

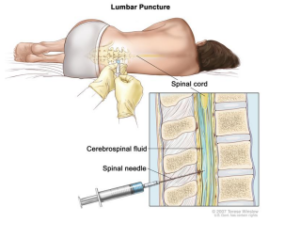
- Lumbar puncture: The removal of a teaspoon of cerebrospinal fluid (CSF) by placing a needle between two bones in the lower spine while the child is sedated. CSF is reviewed under a microscope for leukemia, and chemotherapy is injected at the same time. This is repeated throughout the entire course of treatment so that leukemia cells don’t hide there.
Is childhood AML curable?
Childhood AML is more curable than in adults, and long-term cure rates with modern day chemotherapy may be as high as 80% if your child is in a low-risk group and receives up-todate treatment. Cure rates vary widely depending on which risk group he or she is in. For example, M3/APL responds so well to specific targeted drugs that it is discussed in a separately.

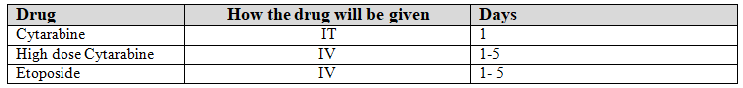
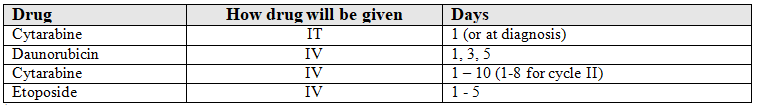 *Subjects with leukemia in the CNS (CNS3) also get IT Ara-C twice weekly until CSF is clears.
*Subjects with leukemia in the CNS (CNS3) also get IT Ara-C twice weekly until CSF is clears.