What is Acute promyelocytic leukemia (APL)?
APL is a cancer of the blood in which the bone marrow makes too many immature promyelocytes (a kind of white blood cell). Blood is made in the bone marrow where white blood cells pass through various stages as they mature in the marrow. In APL there is a genetic defect in a rogue cancer cell, which causes it to multiply and fill up the bone marrow with immature cancerous white blood cells (blasts). This prevents normal white cells, red cells and platelets from being formed, leading to anemia and easy bleeding. The bleeding is worsened by substances in the APL blasts, so it is extremely important to start treatment urgently.

What are the signs of APL?
- Easy bruising or bleeding.
- Petechiae (dark-red spots under the skin).
- Weakness, feeling tired, or looking pale.
- Loss of appetite.
What causes APL?
Although we know the genetic defect usually present in APL blasts, we do not know what causes this. Commonly there is nothing in the environment or diet, and it is not inherited so other family members should not be at risk. It is also not infectious so it cannot be passed onto other family members or neighbors.
How is APL diagnosed?
We may suspect the diagnosis from the blood count but the tests described below will confirm it
- PPhysical exam and history: An exam of the body to check or signs of disease,
- Blood tests: such as complete blood count (CBC) tells the number and type of each blood cell, and blood chemistry and clotting studies help in initial care and to avoid complication
- Bone marrow aspiration and biopsy: Removal of liquid bone marrow and a small piece of bone by inserting a needle into the hipbone while sedated provides material for a pathologist to look at under a microscope to confirm the diagnosis. APL blasts have a distinct appearance with large bright red granules/rods as seen below (FAB Classification M3).
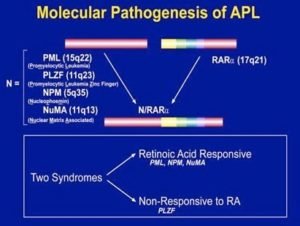
- Additional tests include flow cytometry to look at markers on the surface of leukemia cells, and genetic testing of APL blasts for the defect PML/RARA. Almost all patients will have it in their blasts and PML/RARA levels can be monitored in blood or marrow to see if the leukemia has cleared completely.
Is AML curable?
APL is a subtype of Acute myeloid leukemia (AML), but is very different because it is very sensitive to some highly effective targeted treatments. Long-term cure rates are 80% or higher, with little or no long-term effects. APL is rare with only 5000 cases per year diagnosed in the whole of India, so it is important to be treated by experts familiar with this condition.